Skin rejuvenation, via rhytide reduction, is one of the most requested services in the medical aesthetics field. If we are to properly address wrinkles, we first need to understand the physiology and histology of the Dermal-Epidermal Junction. After all, this is where wrinkles are born and grow. With this understanding, we can then prescribe effective clinical treatments and home care, which should be addressing the DEJ if wrinkle reduction is the goal.
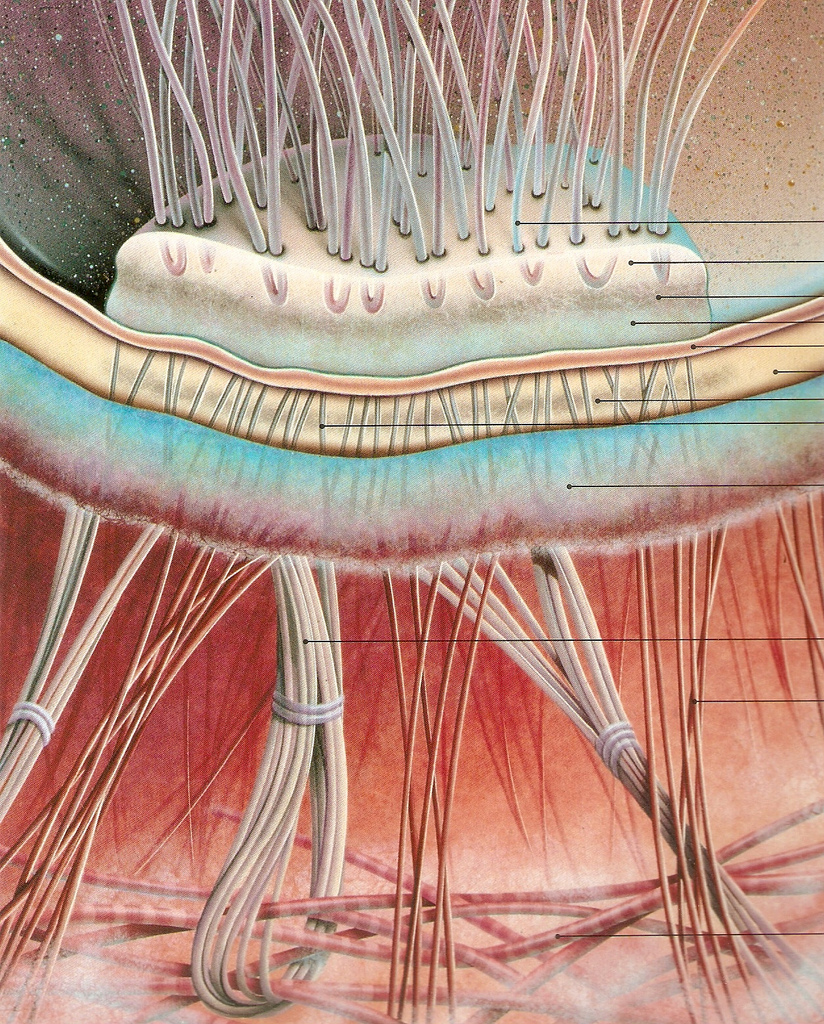
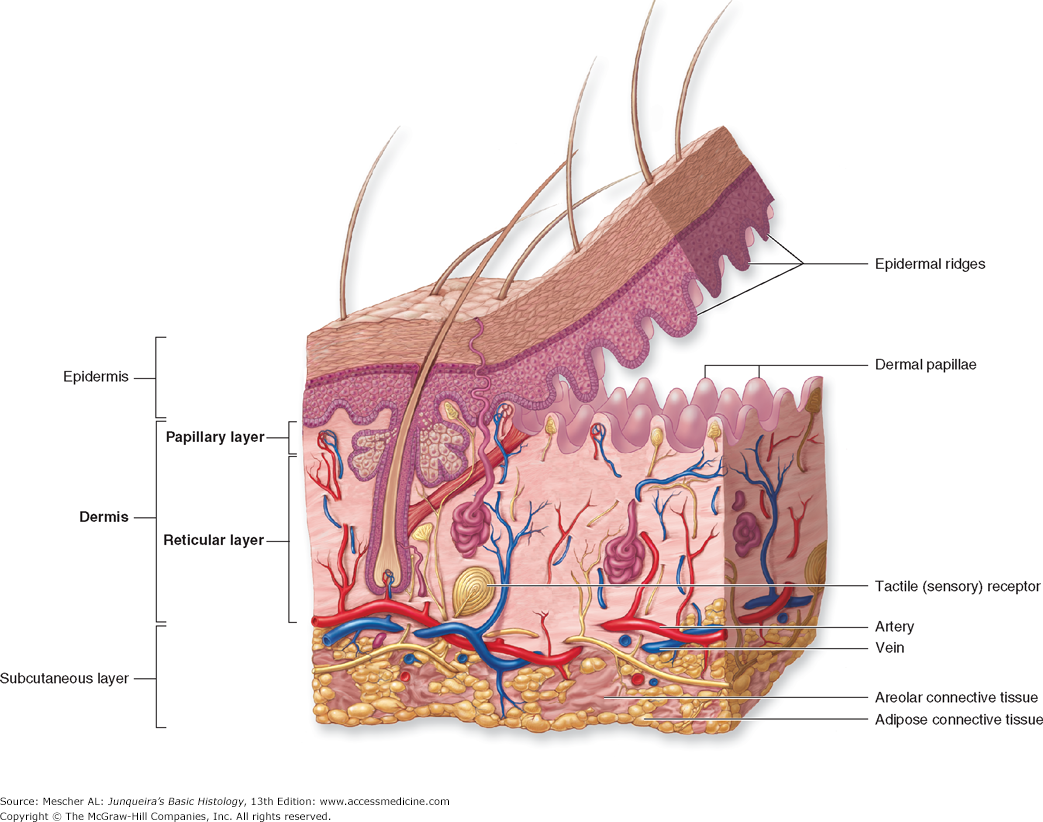
The DEJ is is made up of four regions:
- The basal epidermal cell membrane which contains: keratinocytes, melanocytes and Merkel cells.
- The lamina lucida is traversed by anchoring filaments rich in laminin that adhere to keratinocytes to form an adhesion structure.
- The lamina densa is mostly composed of type IV collagen. It is thicker in men than women.
- The fibril zone has anchoring fibrils that are made up of type VII collagen, connecting the lamina densa to the papillary dermis.
It is a loss of adhesion in the four regions of the DEJ that causes a wrinkle. Loss of adhesion could be a result of intrinsic and extrinsic sources. A thorough medical and lifestyle consultation should illuminate where the client can intervene to improve her own DEJ through lifestyle modifications. However, once a wrinkle has started, it’s like a snag in panty hose, it will just keep going.
Microneedling is the most effective way to strengthen and repair adhesion in the DEJ in a clinical setting. We already know that reticular fibroblasts are not responsive to microneedling. It is the stimulation of the cells (keratinocytes) leading down to the DEJ that induce the wound healing response responsible for skin rejuvenation. Collagen type VII is produced by the keratinocyte and is responsible for the visual improvement we see in the skin. The keratin gene, KTR5, produced by the keratinocyte, is also up-regualted post microneedling and aids in dermal-epidermal adhesion.
Prescriptive skin care products can also aid in the repair of the DEJ by giving the cells what they need to regulate themselves. Omega 3 & 6, ceramics, squalene, phospholipids and antioxidants are all required for optimal keratinocyte function.
We do not need to pull blood or administer an aggressive treatment to stimulate and repair the DEJ. Direct injury of the dermal cells is not necessary. The keratinocyte produces collagen VII and expresses genes necessary for repair and adhesion of the DEJ. A less is best approach with microneedling will still produce effective results, while minimizing complications and pain. If we can understand and address the dermal-epidermal junction, we will be giving our patients the best possible treatment with the best possible outcomes.
References:
https://www.ncbi.nlm.nih.gov/pubmed/1097542
https://www.sciencedirect.com/science/article/pii/S0955067497801184
https://www.sciencedirect.com/science/article/pii/S0022202X15436504
https://www.sciencedirect.com/science/article/pii/S0022202X15404828
https://ghr.nlm.nih.gov/gene/KRT5